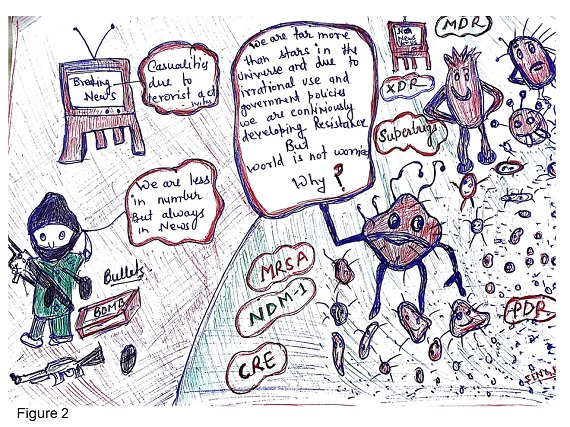
“Antibiotic resistance bacteria should be considered as micro terrorist. They are silently killing human and modifying the normal bacterial flora to resistant one through genetic transfers”
Antimicrobial resistance is an emerging public health threat worldwide but nowhere its socio-economic effect is as stark as in developing countries. Centre for Disease Control and prevention (CDC), Atlanta, USA published a data on annual deaths due to antibiotic resistance (AR) in European Union, India, Thailand and USA; 25000 deaths per year, 58000 babies died in a year, 38000+ deaths per year, and 23,000+ deaths per year respectively [1]. Another report found high crude infectious disease mortality rate in India i.e. 416.75 per 100,000 persons and considered misuse of antibiotics along with suboptimal dosing, environmental contamination etc. are the major drivers for incidence of AR [2]. Sub-optimal rapid diagnostic tools are also one of the risk factors for development of antimicrobial resistance (AMR) [2]. In most of the developing countries, over-the-counter access to antibiotics and growing antibiotic use in the animal husbandry sector without any professional oversight, are other factors resulting emergence of AMR. Beckel et al reported global antimicrobials consumption in food animal production was 63,151 (±1,560) tons in 2010 and projected to rise by 67%, to 105,596 (±3,605) tons, by 2030. They also observed China, United States, Brazil, India, and Germany had largest shares of global antimicrobial consumption in food animal production [3].
AMR is not just a health problem but an economic burden too. The overall cost, both in terms of lives lost and money wasted, is too great to be ignored and the whole world must come together to agree on a common solution. Study performed by Roberts et al on evaluation of the economic and health outcomes of AMR found that the costs were considerable and in sensitivity analysis, they observed medical costs ranged from $18,588 to $29,069 per patient [4]. According to Economist Jim O’Neill, at per current scenario, world population by 2050 will be between 11 million and 444 million lowers than it would otherwise be in the absence of AMR bacteria. This reduction in population and the morbidity impact would lead to reduction of world Gross Domestic Product (GDP) to 0.06% and 3.1%, depending on the scenarios. As these GDP losses are annual and compound over time, resulting in a cumulative loss that ranges between $2.1 trillion and $124.5 trillion [5]. Based on these data it has been speculated that resistance to antibiotics is as great risk to public safety as terrorism, in the world, and If left unaddressed antimicrobial resistance will become an even greater threat to mankind than terrorism.

68th World Health Assembly highlighted the need to contain ARB and endorsed a global action plan to tackle AMR, including the most urgent drug resistance trend. Worldwide data coming from the AMR projects on trends of AR and their mechanism are mostly limited to human subjects. There is substantial lack of data from animals and plant sector. That raises the question to microbiologists across world: Are we doing enough to counter AMR issue? Or Government should do more on this socio-economical problem (Figure 1). Former US President Obama in 2016, nearly doubled the federal funding for combating and preventing antibiotic resistance to more than 1.2 billion USD. Interestingly, Sweden is the only country where very less cases of antibiotic resistance have been reported due to their strict policies and political will. In developed world there is a restriction on sale of over the counter antibiotics and are prescribed only after antibiotic sensitivity tests (AST). While in majority of the developing countries, especially in India there is no such restriction on purchase of antibiotics without any prescription. In developing countries, governments should open AST centres at district level, to help clinicians for prescribing right antibiotics. Now a days automated instruments are available that can perform ASTs and quick identification in few hours. Doctors can use these identification reports before prescribing antibiotic to the patients. Government should give additional special budget to fight with AMR. This budget should be utilized in setting AST centres at district levels and for social awareness programmes.
To conclude, antibiotic resistance bacteria should be considered as micro terrorist. They are silently killing the human and modifying the normal bacterial flora to resistant one through genetic transfers. Antibiotic resistance and terrorism are two major problems in developing countries and it should be kept in top most priority on the government's national risk register along with other emergency conditions (Figure 2). A strict vigilance by drug regulatory bodies is need of hour to safeguard against powerful antibiotics being sold over the counter and to phase out the use of antimicrobial growth promoters in livestock. Strict implementation of policies, regular revision of strategies, routine surveillance and monitoring of use of antibiotics in human and animal health sectors and release of funds for development of newer antibiotics are urgently needed to combat the rise of AMR.
Acknowledgement: Dr Avinash Singh is thankful to DST-SERB-NPDF fellowship (PDF/2017/000654) for providing the funds.