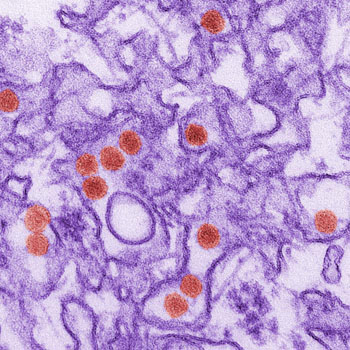
As the global spread of the Zika virus continues, efforts are underway to halt the disease’s transmission. While no licensed therapies or vaccines to protect against the Zika virus are currently available, new research published in the journal npj accines demonstrates how a synthetic DNA vaccine approach successfully protected against infection, brain damage and death caused by the mosquito-borne Zika virus in vivo.
In this preclinical study, 100 percent of the animal models were protected from Zika after vaccination followed by a challenge with the Zika virus. In addition, they were protected from degeneration in the cerebral cortex and hippocampal areas of the brain, while the other cohort showed degeneration of the brain after Zika infection.
This study is the first of its kind to analyze a vaccine in an animal model that is susceptible to the disease, providing information regarding the protective impact of the immune response in susceptible individuals. Prior studies of the Zika virus have tested vaccines in animal models that are naturally resistant to Zika. This study extends these prior research studies in an important manner.
In this latest study, Weiner and colleagues demonstrated how a synthetic DNA vaccine expressed specific antigens for Zika in vivo. They observed that this novel vaccine generated robust antigen-specific antibody and T cell responses that neutralized the virus in preclinical animal models. Moreover, they found that the vaccine provided protection against the disease and death in animal models while also being neuroprotective, meaning that the disease was unable to spread to the brain. This is especially important given the risk that infants born with the disease have of developing microcephaly, a birth defect resulting in an abnormally small head and that may prevent the brain from developing properly.
One important aspect of Zika and many other mosquito-borne diseases is that not everyone infected with the virus will actually become ill as a result. With Zika, only about 20 to 25 percent of individuals with the virus are actually impacted by the disease, according to previous studies from the U.S. Centers for Disease Control (CDC). However, there is no way to know for certain who will be at risk for illness due to the virus, which is why it was crucial for this study to examine how a vaccine would operate in an infected, symptomatic host.
This Zika vaccine is being developed in collaboration between Inovio, The Wistar Institute, and GeneOne Life Science Inc. and is currently being tested in two human clinical studies. Before the end of 2016, Inovio expects to report phase I data from the first 40-subject study being conducted in Miami, Philadelphia and Quebec City. In August, the companies also initiated a second study in 160 subjects in Puerto Rico. The CDC estimates that Zika will infect more than 25 percent of the Puerto Rican population by the end of the year, creating the potential for this study’s placebo-controlled design to provide exploratory signals of vaccine efficacy in 2017.
A total of nearly 4,000 cases of Zika infection have been reported in the United States alone, according to the CDC. While most of these are travel-associated cases, more than 100 cases of Zika infection originating within the United States have been reported. Globally, more than 60 countries have reported mosquito-borne transmission of the disease.