Genomic testing of biopsies from patients with deadly, treatment-resistant cancerous blood syndromes called histiocytoses allowed doctors to identify genes fueling the ailments and use targeted molecular drugs to successfully treat them.
Researchers from the Cincinnati Children’s Cancer and Blood Diseases Institute report their data in Journal of Clinical Investigation Insight (JCI Insight). They recommend the regular use of comprehensive genomic profiling at diagnosis to positively impact clinical care, as well as rigorous clinical trials to verify and extend the diagnostic and treatment conclusions in their study.
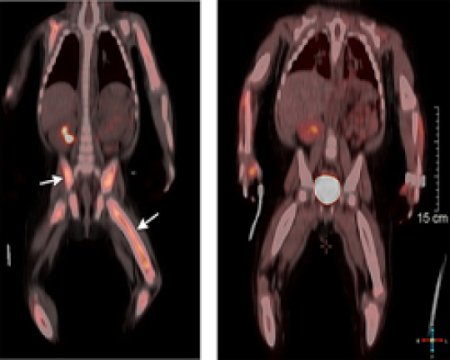
Histiocytoses are a group of disorders in which abnormal accumulations of white blood cells form tumors on vital organs, leading to systemic organ damage or death. About half of the patients can be treated successfully with chemotherapy, but others are treatment resistant.
Study authors conducted genomic profiling of biopsies from 72 child and adult patients with a variety of treatment-resistant histiocytoses, including the most common one in children, Langerhans cell histiocytosis (LCH), according to the lead investigator, Ashish Kumar, MD, PhD.
Twenty-six patients with treatment-resistant disease had gene mutations involving either BRAF or MAP2K1 that directly activate the MAP-kinase cancer pathway. Researchers determined such patients would benefit from the targeted molecular therapies dabrafenib or trametinib, which block the MAP kinase pathway. The approved cancer drugs were prescribed off label to the histiocytosis patients.
"In the last year, three patients we treated were infants with disease that was resistant to several rounds of intense chemotherapy. In the past, these children either would have suffered serious complications including death or would have had to endure more intensive treatments and the ensuing toxicities, including the risk of death,” Kumar said. “All three are thriving now on one oral medication that put their disease into remission.
Source: newswise.com