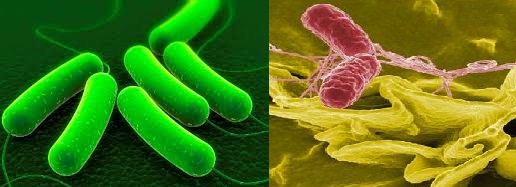
E. coli and Salmonella – the most causative food borne pathogens – "National Threat to Human Health”
E. coli and Salmonella, the two most causative food borne pathogens belongs to same family Enterobacteriaceae, are genus of rod-shaped, Gram-negative, non-spore-forming and facultative anaerobic bacterium. E. coli are normally found in lower intestine of human and all warm blooded animals and benefit their host by synthesizing vit-K2. While salmonella has been found worldwide in both cold-blooded and warm blooded animals, and in the environment.
Salmonella
Food poisoning Salmonella belongs to two paramount causative species - Salmonella enterica and Salmonella enteritidis, responsible for diarrhea, vomiting, and abdominal cramps. They usually are not destroyed by freezing. Ultraviolet radiation and heat acceleration above 75 °C for not less than 10 mins is recommended to prevent proliferation. Every year, approximately 42,000 cases of Salmonellosis are reported in the USA. Because many milder cases are not diagnosed or reported, the actual number of infections may be twenty or more times greater. In Germany, food poisoning infections between 1990 and 2005, cases decreased from approximately 200,000 to approximately 50,000 cases. In the USA, about 40,000 cases of Salmonella infection are reported each year.
Reptiles, such as turtles, lizards, and snakes, carry the bacteria belonging to Salmonella bongori (which inhabits old-blooded animals) in their intestines which can cause intestinal infections. Outbreak of Salmonella Serotype Hartford Infections Associated with Unpasteurized Orange Juice is also reported.
E. coli
E coli dwell in a diverse group of bacteria. Pathogenic E. coli strains are categorized into six pathotypes, associated with Bloody diarrhea, Stomach cramps, Nausea and vomiting as shown below:
- Shiga toxin-producing E. coli (STEC)—STEC or Verocytotoxin (VTEC), most commonly identified in North America is E. coli O157:H7. The other strain of Shiga toxin-producing E. coli is O104:H4, leading to to hemolytic-uremic syndrome (HUS)(HUS). Other E. coli in the STEC group belongs to E. coli O145, O26, O111, and O103, ultimately leads to kidney failure.
- Enterohemorrhagic E. coli (EHEC), associated with foodborne outbreaks, was recognized first in 1982, following an outbreak in the United States of America, can grow in temperatures ranging from 7°C to 50°C, with an optimum temperature of 37°C. Some EHEC can grow in acidic foods, down to a pH of 4.4, and in foods with a minimum water activity (Aw) of 0.95. It is destroyed by thorough cooking of foods until all parts reach a temperature of 70°C or higher.
- Enterotoxigenic E coli (ETEC)
- Enteropathogenic E. coli (EPEC)
- Enteroaggregative E. coli (EAEC)
- Enteroinvasive E. coli (EIEC)
- Diffusely adherent E. coli (DAEC)
Context of India/South East Asia
The term Food-borne pathogens, including food-borne infections, covers illnesses acquired through consumption of contaminated food and to access safe food still remains a major obstacle in large percentage of the people belongs to South East Asian Region (Bangladesh, Bhutan, India, Indonesia, Myanmar, Nepal, North Korea, the Republic of Maldives, Sri Lanka and Thailand) due to increase in rapid population, illiteracy and unstructured economic growth of the countries. Hence a regional strategy must be developed to combat those concerns. Microbiological contamination of food and water has been found a major cause of illnesses and deaths in Bangladesh, India and Indonesia due to hot and humid character of weather. Approximately one million children under the age of five die each year from diarrheal diseases after consuming contaminated food and water. Cholera has been found a major health concern in this region - particularly in Bangladesh and India, where transmission has been found occurred through contaminated foods served by street vendors and even restaurants.
In Thailand, approximately a million cases of acute diarrhea reported each year. Raw or undercooked food and contaminated water and poor environmental sanitation have been found the major causes and children less than five years of age are very prone to be infected.
Countries like India, Indonesia and Nepal lack critical enforcement of health and food safety regulations against street food vendors due to a shortage of health inspectors, inadequate infrastructure and low division staffs.
According to a study from the International Food Policy Research Institute (IFPRI), developed countries are still continue to reject all raw agricultural as well as processed food products produced by South Asian countries.
Only Thailand adopted a training program to improve food safety and hygiene for retailers, restaurants, and other food services through voluntary inspection and certification of food service businesses.
Source of contamination
Ø consumption of unpasteurized (raw) milk, unpasteurized apple cider, and soft cheeses made from raw milk
Ø consumption of water from pool, lake, local pond, contact with cattle or contact with the feces of infected people
Ø consumption of an undercooked hamburger (ground beef meat), dried cured salami or a contaminated piece of lettuce sprouts, spinach, lettuce, coleslaw, salad
(Use of Copper Cast Alloys to Control E. coli O157 Cross-Contamination during Food Processing has been developed and employed recently)
Incidence of Outbreak
- In 1985, an outbreak of Salmonellosis was reported, caused by contaminated pasteurized milk, more than 2% of the 170,000-200,000 people infected suffered from reactive arthritis as a result of their infection in Chicago, USA
- In 1994-2000, E. coli 0111 strain was found in Ground beef, unpasteurized apple, salad, US and Canada
- In 1995, food poisoning affecting 33 people, by Salmonella paratyphi A was vegetarian food, Yavatmal (Maharashtra) India
- In 1998, food poisoning affecting 78 people, by Salmonella enteritidis was identified as the etiological agent, India
- In 1999-2006, E. coli 0129 strain lettuce, lake water, US and Canada
- In 200-01, Salmonella enteritidis (SE) phage type 30 (PT30), a rare strain, was detected in raw almonds, Canada
- Virulent E. coli O157:H7 strain was found in dairy cattle and beef market, Calcutta
- In 2006, Environmental studies documented the presence of Salmonella sp from the hands of butchers as well as abattoir equipment from Punjab. Nearly 8% of eggs and 7% of egg-storing trays from retail markets in Coimbatore were found to be contaminated with Salmonella enteritidis, in Coimbatore, India
- In 2006, Almost 200 people in 26 states were sickened, 31 developed HUS, and three people died, after consuming prepackaged leafy greens, Lettuce, fresh spinach containing E. coli O157:H7, USA
- In June 2006, the BBC reported the Cadbury chocolate manufacturer withdrew a number of products contaminated with Salmonella, which had resulted in up to 56 cases of Salmonellosis in Herefordshire, UK
- In February 2007, the FDA issued a warning to consumers not to eat certain jars of Peter Pan or Great Value peanut butter, due to risk of contamination with Salmonella Tennessee.
- In March 2007, around 150 people were diagnosed with Salmonellosis after eating tainted food at a governor's reception in Krasnoyarsk, Russia. Over 1,500 people attended the ball on March 1, and fell ill as a consequence of ingesting salmonella-tainted sandwiches.
- In 2007, About 150 people were sickened by salmonella-tainted chocolate cake produced by a major bakery chain in Singapore
- From April 10, 2008 to July 8, 2008, the rare Saintpaul serotype of S. enteritidis caused at least 1017 cases of Salmonellosis food poisoning through fresh salsa, such as raw tomato, fresh jalapeño pepper, fresh serrano pepper, and fresh cilantro in 41 states throughout the United States, the District of Columbia, and Canada.
- On January 17, 2009, Salmonella was reported to be found in 46 states in the United States in at least 3,862 peanut butter-based products in company Blakely, Georgia, owned by Peanut Corporation of America (PCA), such as crackers, energy bars, and peanut butter cookies from at least 343 food companies. At least 691 people in more than 46 states became sick, and the Salmonella claimed at least 9 lives as of March 25.
- in 2008-09, two separate food poisoning outbreaks due to Salmonella weltevreden and Salmonella wein in chicken and fish, affecting 34 and 10 people respectively, were reported, Mangalore, India
- On 30 June 2011, the German Bundesinstitut für Risikobewertung (BfR) (Federal Institute for Risk Assessment, a federal, fully legal entity under public law of the Federal Republic of Germany, an institute within the German Federal Ministry of Food, Agriculture and Consumer Protection) heralded that seeds of fenugreek contaminated with E. coli is O104:H4, procured from Egypt were likely the cause of the EHEC outbreak, Germany
- In 2012, Salmonella bareilly, was reported in multiple states mostly in the East, having yet caused no deaths, but many episodes of sickness and some hospitalizations have been linked to the consumption of raw scraped ground tuna product, USA
- In July 2013, 33 people became ill, with two people developing hemolytic uremic syndrome (HUS), after consuming prepackaged leafy greens containing E. coli O157:H7, USA