At an address to the UN in 2016, Margaret Chan, the then director general of the World Health Organisation (WHO), highlighted the issue of antimicrobial resistance, stating that it may “bring the end of modern medicine as we know it”. The global trends of antimicrobial resistance paint a frightening picture for the future of medicine. Although difficult to predict, one report suggests that if something isn’t done soon, by 2050, 10m people may die every year from antimicrobial-resistant infections.
Antimicrobial resistance occurs when microbes (such as bacteria, viruses or fungi) become resistant to drugs commonly used to treat them. The overuse of antibiotics has been widely reported as a cause. But there is another cause that is often overlooked, and that is misdiagnosis.
Misdiagnosis and resistance
Along with other microbes, such as viruses and bacteria, fungi present a significant disease burden worldwide, with an estimated 1.7m deaths a year from serious fungal infections. Several species have become resistant to antifungals, a type of antimicrobial drug used specifically to treat fungal infections. For example, a specific type of fungus, Candida auris, was in the headlines recently after multi-drug resistant infectionswere diagnosed in hospitals around the world. This species of fungus is often misdiagnosed as the less dangerous Candida haemulonii, something which may have contributed to the development of resistance.
Most serious fungal infections occur in hospitalised patients and those with reduced immune responses. When doctors suspect an infection, a sample of blood, or other relevant bodily fluid, is sent to a laboratory for testing.
Due to a lack of fast and accurate diagnostic tests, the prescription of antimicrobial drugs is rarely based on an accurate diagnosis. Consequently, hospital patients suffering from serious fungal infections are often prescribed broad-spectrum antimicrobial drugs (drugs that don’t discriminate between good and bad microbes).
This lack of accurate diagnosis not only causes preventable deaths, but adds to the development of antimicrobial resistance. The more drugs used, the greater the risk of resistant bacteria and fungi spreading throughout the population.
Outdated tests
Bacterial and viral diagnostic tests are continually being developed to meet the need for quicker and more accurate testing. These tests are becoming faster and easier to use. But the field of fungal diagnostics seems to have been left behind.
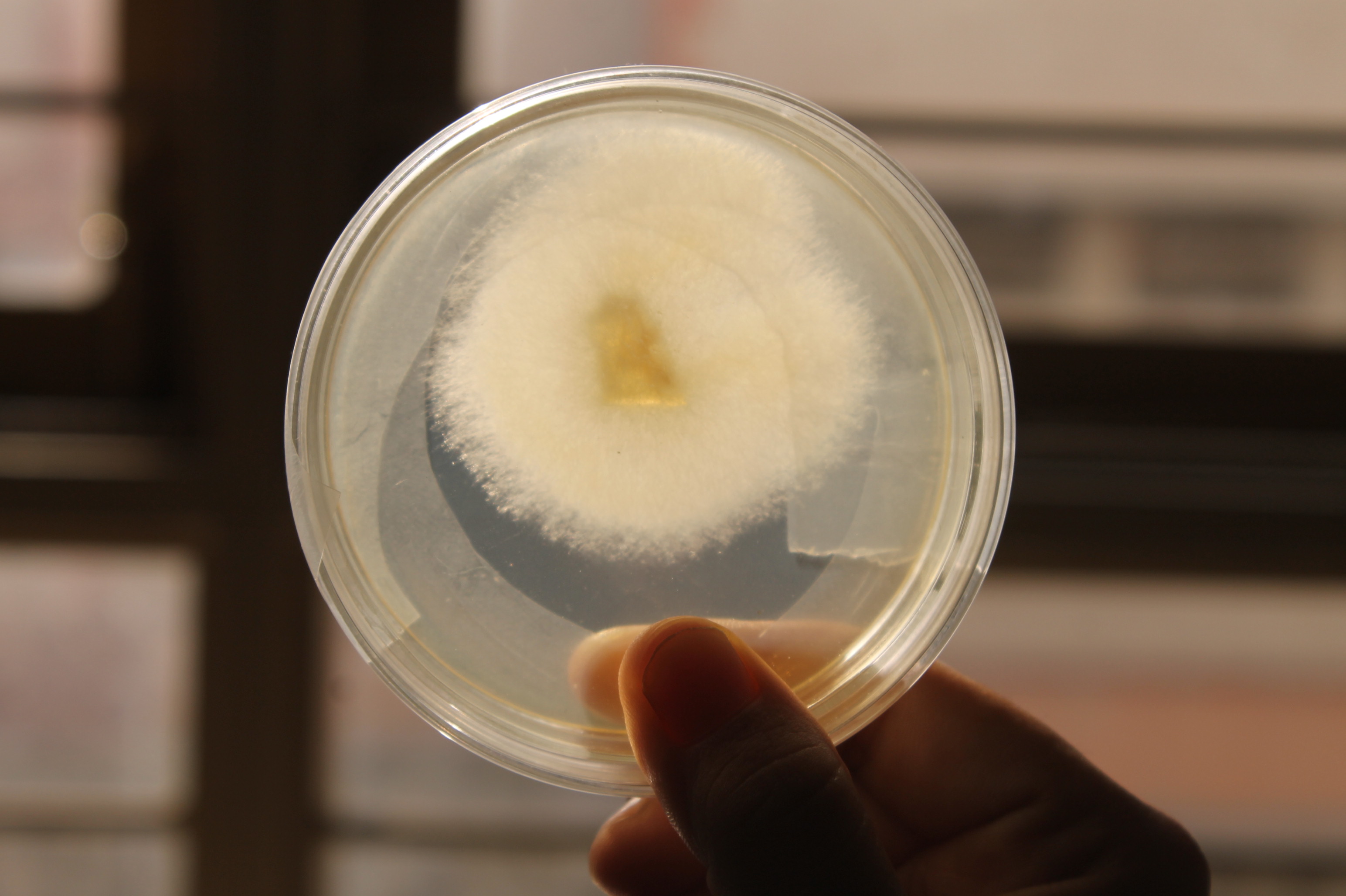
Hospital fungal infections are generally diagnosed using blood culture tests. This involves incubating a sample of a patient’s blood until the fungus grows enough to be detected. Specially trained microbiologists are then needed to determine the species that the patient is infected with. While this technique is used in laboratories worldwide, large blood samples have to be collected from patients and the test can take up to 14 days to complete.
The charity Global Action Fund for Fungal Infections predicts that more than 80% of patients could be saved if specialised diagnostics and antifungals were available everywhere, and were used wisely by doctors. At the moment, though, diagnosis of fungal infections takes too long, requires specialised training and is not accurate enough to meet the needs of doctors.
The future is molecular
Several good alternatives come in the form of molecular diagnostic tests. While blood culture relies on the fungus growing over time, molecular tests detect the DNA of small amounts of fungus. This means that a smaller blood sample is needed and the infection can be detected much earlier. But they still have a long way to go.
Although there are some molecular tests commercially available, they often can’t tell doctors exactly what type of fungus the patient is infected with. The current tests still aren’t reliable enough to be adopted in mainstream clinical diagnosis.
The future of molecular tests is bright, though, with new technologies being brought to the field each year. New tests could be developed to detect fungi and rule out bacterial infections. They could tell doctors what drugs the fungus is resistant to, taking hours, rather than days, and improving the outcome of patients in hospitals across the world.
We need to tackle the underlying issues in order to reduce the number of antimicrobials used globally and slow down antimicrobial resistance. One of these relates to the lack of adequate tests for fungal infections. With a quicker and more efficient diagnostic, doctors will be able to make more informed treatment decisions, minimise the use of broad spectrum antimicrobials and help to combat emerging resistance.
Source: This article published in The Conversation by Ambalika Batra, a post-doctoral scientist at Royal Holloway, University of London.