When Henrietta Lacks, a black tobacco farmer, got admitted in John Hopkins Hospital, she had no idea that she would create such a furor in the scientific world. Henrietta suffered from cervical cancer and had been undergoing treatment under Dr. Howard Jones, a gynecologist who used radium capsules to treat her cancer. Biopsies were ordered to confirm the condition
It was malignant cancer, no doubt which had spread throughout her body. The tissue from her second biopsy was given to Dr. George Gey, director of tissue culture research at Hopkins. No consent was taken from Henrietta. At that time consent was neither required nor customarily sought. Gey had been trying from a long time to create an ‘immortal’ cell line which would supply researchers with an endless supply of cells which would not die, hence giving a new edge to the method of study of cell function. Research costs would also reduce drastically.
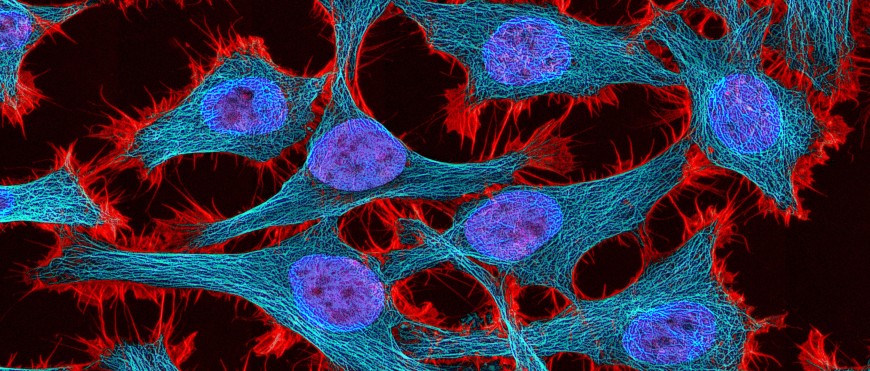
With HeLa (Gey’s naming method based on the donor’s initials), this seemingly impossible goal was accomplished. Technicians in Gey’s lab thought that these cells too would die or grow for some time before dying. But they multiplied uncontrollably duplicating in 24 hours.
Henrietta Lacks died on 4th October 1951. The same day Gey appeared on a T.V. show ‘Cancer can be conquered’ and announced his breakthrough- the first human cell line. HeLa cells became the workhorses of labs worldwide.
Dr. Jonas Salk in Pittsburg Medical School had been trying to produce a vaccine for the polio virus which was killing or paralyzing millions worldwide. HeLa cells were perfect for Dr Salk to test his vaccine on. By 1955 he had successfully created the vaccine which would nearly eradicate the feared disease.
HeLa cells were astoundingly robust. They could be shipped and stored easily. Soon they started getting bought and sold commercially creating an industry of millions of dollars. Dr. Gey had given away the cell lines that he had created without making money out of it. But he never imagined that these cells would become an indispensable part of research leading to drug production for cancer, Parkinson’s, Flu, besides being tested on in space, tested for human sensitivity to glues, dyes, cosmetics and a variety of other products.
The Ethics Issue
While her cells created an industry of millions of dollars. Henrietta Lacks’ family remained in poverty. They were ignorant of the ‘immortal’ cells that their mother had donated unknowingly. In the early 1970s researchers started contacting the family for blood samples. HeLa cell batches had got contaminated and researchers wanted information on the Lacks family genetics to replace the contaminated cells. Henrietta’s family was aghast and confused. They felt that they had been cheated and their mother’s cells misused. They wanted justice.
The Case of John Moore
The 1990 case of Moore vs. Regents of University of California was a landmark case on use of tissues of patients without consent. John Moore, a leukemia patient accused his doctor Dr. David Golde of using his spleen tissue to create a cell line without his consent. This cell line replicates itself indefinitely and led to production of nine pharmaceutically significant substances including the granulocyte-macrophage colony-stimulating factor which was commercialized by Golde and UCLA. Moore had signed consent forms which allowed his tissues to be used for research. But he had explicitly signed against their commercial use. He felt that justice was due to him and filed suit.
In the landmark judgment, the California Supreme Court ruled that a hospital patient's discarded blood and tissue samples are not his personal property and that individuals do not have rights to a share in the profits earned from commercial products or research derived from their cells. The court said that ruling in Moore's favor might "destroy the economic incentive to conduct important medical research."
Henrietta Lacks’ family finds closure
In 2010, journalist Rebecca Skloot released her book ‘The immortal life of Henrietta Lacks’ which became a best-seller bringing this story before the world. After about six decades the National Institute of Health (NIH) acknowledged her role in furthering scientific research in 2013 and made a deal with her family. The HeLa genome would be available in full only to researchers who apply and are selected by a panel which would include two members of the family. Though excluded from commercial profits this was an ethical victory for them.
Tissue rights in India
The Institutional Review Board (IRB) or the Institutional Ethics Committee (IEC) established by the Indian Council of Medical Research (ICMR) governs laws on ethical biomedical research on human subjects. Though consent is routinely sought before tissue donation, still in India, there remains more scope for creating awareness on the ways that genetic and tissue information can be used or misused for commercial purposes.