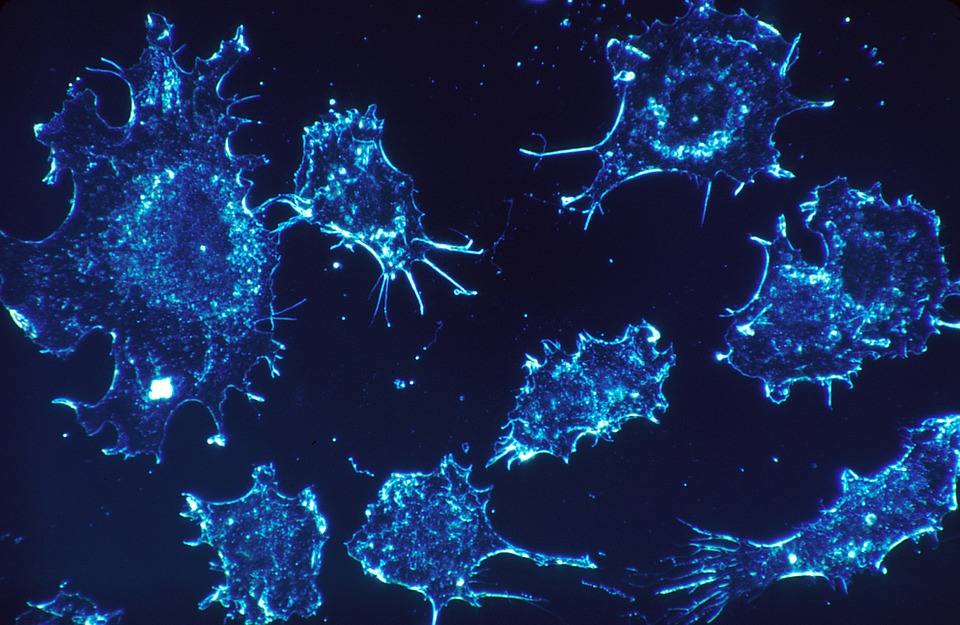
Cells, the units of life that compose our bodies, are able to make copies of themselves to help us grow, fight disease and recover from injuries. As cells divide to generate new cells, sometimes errors are introduced. These errors are called mutations and they shape the fitness of an individual cell in the context of the many cells in our body, similarly to how the shape of a grain of sand dictates if it passes through a sieve: while most mutations are harmless, some can kill cells, or even worse, trigger cancer.
In the early 1950’s it was proposed that two of these mutations are needed for cancer to start1,2 and this prevailed as the current of thought in the cancer field.Since we have two “good” copies of each gene, completely destroying a gene implies that both copies have to acquire inactivating mutations (two-hits). Destruction of genes which guard the genome (tumor suppressors) or mutation of genes that directly cause cancer (oncogenes), both of which are commonly referred to as cancer “drivers”, is therefore unlikely. The probability of these events occurring in our lifetime is very low, which contrasts with the high rates of cancer incidence. Now, we have discovered that cancer might arise more easily than previously thought: by combining evolution of yeast cells and human cell culture experiments we were able to show that a single mutation suffices to accelerate cancer. The experiments mimic an early event during cancer development, the acquisition of genetic instability – which is characterized by a faster accumulation of mutations and genomic changes which can themselves disrupt cancer tumor suppressor genes or activate oncogenes. Hence, by dialing up the speed at which mutations are generated, it is more likely to randomly hit genes that upon mutation cause cancer.
So far it has been difficult to identify when and where genetic instability arises, either because the tumor samples carry many different mutations and represent a late stage of cancer development, or because studies with model organisms are focused on inactivation of specific genes. This new work3 started from a provoking question posed to me by my mentor, Andrew Murray: “If we let cells choose, how do stable cells evolve into cancer cells?”. Catching the initial transition from genetic stability to instability was the crucial goal, and this was done by selecting cells that are able to survive different drugs, each survival step requiring the inactivation of a “tumor suppressor” gene. Mimicking two important aspects of cancer development, the inactivation of cancer suppressors and the acquisition of drug-resistance, we allowed the cells to choose how to evolve accelerated mutation rates. Surprisingly, instead of the predicted two-hits, a single heterozygous mutation (a mutation in one of the two copies of a gene) was the favorite route to evolve instability. This means that, similarly to the famous anime show “One-punch man”, where the hero defeats his enemies with a single-hit, cancer might start with a single mutation.
This contradicts the prevailing thinking current in the field, which states that two inactivating mutations are required for cancer onset1: sincea heterozygous mutation in a single gene suffices to trigger genetic instability, and we predict that cells have 200 such genes, it is very probable that cells turn-on the ability to mutate faster. Once mutating faster, then the chance of hitting tumor suppressors and oncogenes, and genes that favor metastasis or drug resistance, becomes much higher, accelerating cancer development.Hence, this work suggests that a single heterozygous mutation, in one of a large number of genes, is an easy way for cells to acquire a “super-mutator” power that allows cancer to progress faster. From the basic scientific standpoint: similarly to what was shown in bacteria, which dial up their mutation rates in adverse environments, for instance to survive antibiotics, eukaryotic cells also have pedals (genes) that accelerate the speed of evolution, allowing them to escape growth control.These instability genes, relics of a time when single celled organisms needed toadapt to changing environments over evolutionary time, can be detrimental and harming when mutatedin a multicellular organism where uncontrolled cellularproliferation leads to cancer. It is possible that these genes evolved secondary functions that are important for multicellular organismal development, and are therefore essential for metazoans, albeit their role in instability. In collaboration with a research group lead by Ricardo M. Pinto, at the Center for Genomic Medicine (Massachussets General Hospital) we were able to test if the homologs of instability genes we found in yeast worked similarly in human cells: and they did, 5/6 genes tested gave rise to genetic instability when inactivated. We found a total of 57 human instability genes, 47 of which have not been previously implicated in cancer and require further studies. Moreover, many of these genes do not have a known direct function in genomemaintenance, which reveals that other cellular pathways, such as metabolism and protein quality control, can be compromised to cause instability.
Another idea, that I will explore in the future, is that different types of cancer require different instability types (and genes), during different stages of development: since not all tissues express the same genes, I hypothesize that different targets act locally to initially start cancer, and later during metastasis and treatment resistance. For this I will develop experimental evolution systems in organoids (cellular arrays that recreate tissues and organs) and animal models, where I can test the role of instability in different cancers, elucidating for which stages instability is more relevant and how does it interfere with different cancer treatments.
Genetic instability also has implications on cellular aging: it is known that as a cell divides, the speed at which its genetic material mutates, as well as chromosomes shorten and structural rearrangements occur, increases. However, the causality of these events is not well established: is it that instability is a consequence of cellular aging and the cellular inability to repair itself, or is instability triggering senescence? During my doctoral work I discovered that unicellular organisms are able to replicate without exhibiting aging, and it might be that further studying these cells in aging and non-aging inducing environments iskey to answering this question. Therefore, I plan to establish my own research group using experimental evolution systems to explore genetic instability in the context of aging and cancer development. In the long-term findings on what controls the speed of cellular evolution might lead to targeted therapies that delay genetic instability in specific cancer types and prolong human healthy lifespan.
References
1 Nordling, C. O. A new theory on cancer-inducing mechanism. Br J Cancer7, 68-72 (1953). 2 Knudson, A. G., Jr. Mutation and cancer: statistical study of retinoblastoma. Proc Natl Acad Sci U S A68, 820-823 (1971). 3 Coelho, M.; Pinto, R.M.; Murray, A.W. Heterozygous mutations cause genetic instability in a yeast model of cancer evolution. (Nature, 2019).